procedure / hip and knee Compression of the external popliteal sciatic nerve (spe), restless leg syndrome (rls)
Compression of the external popliteal sciatic nerve (spe), restless leg syndrome (rls)
Neurolysis of the sciatic popliteal (or peroneal) nerve, restless leg syndrome
Anatomy:
The external peroneal nerve is situated behind the femur at the neck of the peroneus. It derives from the division of the sciatic nerve into the superficial peroneal nerve at the neck of the peroneus (the fibula) and the tibial nerve (internal popliteal). The peroneal nerve runs through the long and short peroneal muscles. It finishes under the skin on the backside of the foot.
It has a motor function for the front and side muscles in the leg and on the back of the foot. It has a sensory function on the front side of the leg on the bottom half of the leg, on the side of the foot and at the first space between the phalange and other toes and on the top of the last toes.
Description and Symptoms:
The compression of the peroneal nerve leads to motor deficit when walking. The foot falls downwards and requires effort to lift (steppage foreshadowing paralysis, foot drop) or difficulty in raising the toes. The first stage is often painful (night pains with variable intensity until disappearing or improving): at the knee (sensation of tightening or a touniquet); around the top of the foot or near the thigh (paresthesias, tingling), burning sensation in the leg, the impression of having heavy legs (the knee does not hold strong or feels unstable), ankyloses or, on the opposite (“restless leg”). Often, there are cramps in the thigh or the calf or cramps in the back of the knee (cracking knee) or the calf, even if these are old cramps and occur when effort is exerted. Pain can resemble lumbar sciatica. It can follow the path of sciatica or there can be pain in the knees, pain in the backside or pain in the knee and the ankle (associated Tarsal Tunnel syndrome). Sometimes, the patient (as with Tarsal Tunnel) is examined for vascular vein pain (varicose veins or insufficient circulation in the veins). The Doppler ultrasound is negative (no phlebitis).
This compression is common in men and is induced when one is sitting for an extended period of time, on the knees or with legs crossed and/or after surgery. Diabetes, thyroid condition, rheumatoid arthritis all favor this syndrome.
Diagnosis:
During the clinical examination, there may be a deficit in bending the foot or toes backwards. Hypoesthesia presents on the external front part of the leg, on the back top of the foot. This irritable syndrome of the peroneal neck or lower down involves pain and clinical symptoms.
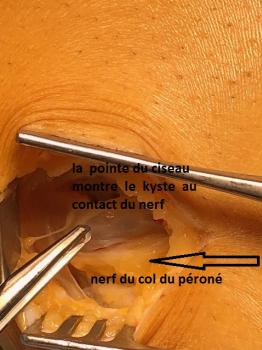
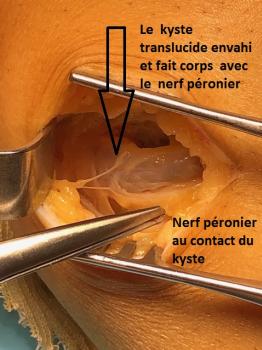
An ultrasound or MRI can rule out the presence of an internervous cyst or a lumbar MRI to rule out a herniated disk or compression of a nerve in the back. Standard x-rays are necessary to seek out other causes. An electromyogram allows for confirming or infirming the diagnosis of tunnel compression (seeking out a radicular involvement or other neuropathy) and indicates how to proceed, even if the electromyogram turns out normal.
Indeed, all these exams can be normal or show anomalies which cannot be interpreted, a fact which often leaves the patient in a state of hopelessness.
Treatment:
Treatment is first medical: first the elimination of aggravating factors, functional physical therapy and wearing a brace in cases of serious steppage, corticosteroid infiltrations of the neck of the peroneus. If medical treatment fails and diagnosis is still uncertain, we will propose neurolysis of the peroneal nerve.
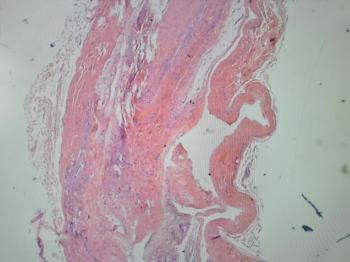
Surgery, aimed at freeing the peroneal nerve from its compression in the aponevroseum of the front of the leg —sometimes to remove an intranervous cyst (cystic schwannoma)— is performed under general or local anesthesia.
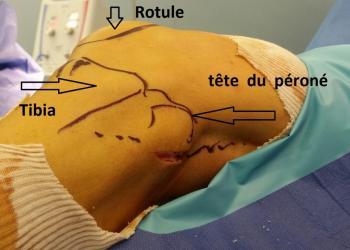
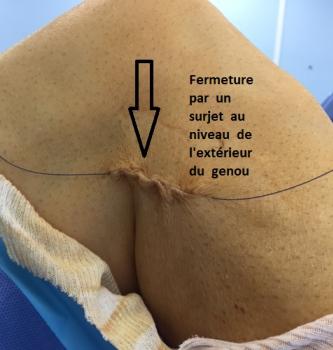
The patient is placed on his/her back with a cushion under the opposite side of the rear end. The surgeon then makes an incision centered on the head of the peroneus.
Free article pubmed : Unusual entrapment... Treated 115 cases by neurolysis P.cottias; DOI: 10.1016/j.otsr.2022.103485.
Hospitalization & Recovery:
Hospitalisation can usually be ambulatory, sometimes a few days, depending upon the situation. Sensory and motor recovery can be long: 18 months to 2 years.
Wearing orthotics to raise the level of the foot is prescribed as necessary.
Regular follow-up appointments will be set up.
Complications:
The most frequent:
The initial regeneration of the nerve can produce transitory symptoms such as numbness or hypoesthesia of the heel and/or toes (even hyperesthesia). These symptoms should disappear, slowly but surely, over a period of several months…(except in diabetic patients whose recovery can last longer)…
Hematomas: as with all surgery, there is a risk of a hematoma, which usually resolves on its own through reabsorption. In exceptional cases, an evacuation puncture or surgical drain may be necessary.
Rare:
Deep infection is possible. It may warrant new surgery and extended treatment with antibiotics. It is strongly recommended to abstain from smoking or consuming other substances during the healing period as tobacco significantly increases the risk of infection.
Algodystrophy (otherwise known as Complex Regional Pain Syndrome (CRPS) and Reflex Sympathetic Dystrophy Syndrome) is a painful, inflammatory phenomenon that is still not well understood. It is treated medically and can last for several months (even years), requiring specific care with adapted rehabilitative physical therapy, complementary testing and sometimes pain management. It is unpredictable in its appearance, its evolution and its potential consequences.
Nerve damage due to persisting inflammation, neuropathy of the external popliteal sciatic nerve or due to perioperative fibrosis causing adhesions;
Other: compartment syndrome, arterial vein wound, phlebitis, pyoderma gangrenosum…
Keywords:
External Popliteal Sciatic Compression — peroneal nerve — fibula —foot drop— motor deficit—loss of sensation in the knee—steppage gait—knee cramps—thigh cramps—calf cramps—restless legs—lumbar sciatica—herniated disk—infiltrative test with corticosteroids—Tarsal Tunnel—varicose veins—insufficient vein circulation—phlebitis—algodystrophia—CRPS—complex regional pain—reflex sympathetic dystrophy—fibroyalgia.