procedure / ankle Tarsal Tunnel Syndrome (TTS) – Distal Posterior Tibial Neuralgia
Tarsal Tunnel Syndrome (TTS) – Distal Posterior Tibial Neuralgia
Anatomy:
The posterior tibial nerve is situated behind the ankle and runs through the foot, through a fibrous tunnel behind the internal malleolus, inserted on the calcaneal tendon, on the bone of the foot, connecting the calf muscle, the triceps surae muscle. The tarsal tunnel is a fibro-osseous tunnel : the distal posterior tibial nerve and its branches —nerves including the calcaneal, the medial and lateral plantar—pass through it as they wind around the medial malleolus into the foot.
Description & Symptoms:
Tarsal Tunnel Syndrome is rare and clinically similar to Carpal Tunnel Syndrome, which is more frequent. The symptoms are neurological: paresthesia, tingling, burning sensations at the bottom of the foot inside spreading to sub-malleol or retro-malleol pain, spreading up to the calf area with sensations such as numbness, “heavy foot” or the impression of “walking on cotton”…It can present as Achilles tendinitis or plantar aponeurosis, plantar fascia, or Sever’s disease (calcaneal apophysitis). It can be associated with plantar pain in the first phalanges of the foot (pain at night, with variable flare-ups, subsiding, feeling better, cracking the ankle).
In advanced cases, the patient can have paralysis in the toes (difficulty to spread the toes out or bend them).
These symptoms can occur during or usually after walking or sports, sometimes waking one up at night with a sensation of tightness or a tourniquet squeezing). There is sometimes a history of foot cramps, calf cramps or cramps in the toes or foot.
It can be associated to a compression at the knee.
Diagnosis:
During the clinical examination, Tinel’s test (light percussing on the nerve) is performed behind the malleolus and on the side of the foot (flexed back). Here we sometimes observe hyperesthesia or hypoesthesia (a loss of sensation) in the retro-malleol, plantar and toe areas. There are sometimes motor symptoms with numbness or tingling sensations (paresthesia) in the interosseals (tested by placing a piece of paper between the toes) or difficulty bending toes.
Sometimes, these signs are attributed to phlebitis or circulation deficiencies, varicose veins and yet the echodoppler test used by vascular surgeons or angiologists finds no vascular anomalies (the veins function normally, there is no phlebitis or thrombosis).
Thus, the diagnosis is chiefly clinical.
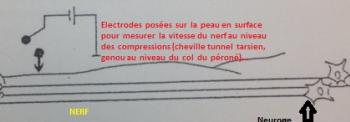
The electromyogram can confirm the diagnosis or a diagnostic test with cortisone infiltration can do so.
An ultrasound or MRI can be used to seek any compression (perineural edema or a change in the nerve volume in the area of the Tarsal tunnel or a compressive cyst). It will be necessary, in any case, to perform standard radiology to seek any other cause (arthritic deformation of the foot…) and eliminate any spinal cause (herniated lumbar disk). All exams can be normal or show anomalies which cannot be interpreted…which often exasperates the patient.
Diabetes, thyroid condition, polyarthritis, rheumatoid arthritis and other conditions can lead to this syndrome.
Treatment:
The first line of treatment is medical (rest, AINS, ice, support socks…) and cortisone infiltrations if the EMG is negative. In case of a positive EMG, it is dangerous to proceed to infiltrations due to the risk of post-operative infection.
In the event that medical treatment fails and the diagnosis is certain, neurolysis (decompression) of the plantar (posterior tibial) nerve will be proposed.
Surgery aims at liberating the entrapped nerve from its ligamentary compression (as in Carpal Tunnel syndrome). It is performed under general or local anesthesia.
Patients are usually lying on their back and the surgeon makes a small internal retro-malleol incision.
Free article Pubmed : Unusual entrament... traeted in115 cases by neurolysis...P.cottias
DOI: 10.1016/j.otsr.2022.103485
Hospitalization & Recovery:
Hospitalization can be ambulatory or last a few days, depending upon the situation.
The ankle can be immobilized with a horseshoe boot (with the foot turned downwards) or a brace for 15 days. One can put weight on the foot during this period of immobilization.
Complications:
The initial regeneration of the nerve can produce transitory symptoms such as numbness or hypoesthesia of the heel and/or toes (even hyperesthesia). These symptoms should disappear, slowly but surely, over a period of several months…(except in diabetic patients whose recovery can last longer)…
The most frequent:
Hematoma: as with all surgery, there is a risk of hematomas that are generally absorbed on their own. On exceptional occasions, evacuating puncture or surgical drainage is necessary.
Phlebitis can occur despite anticoagulant treatment. This is a blood clot that forms inside leg veins with the danger of migrating and leading to pulmonary embolism.
Scar tissue adhesions are possible and would require physical therapy and care.
More rarely:
Deep infection is possible. This may require additional surgery and extended treatment with antibiotics. Smoking is strongly advised against as is consuming other toxic substances during the healing and scarring process as tobacco increases the risk of infection, phlebitis and scar formation troubles.
Algodystrophy (otherwise known as Complex Regional Pain Syndrome (CRPS) and Reflex Sympathetic Dystrophy Syndrome) is a painful, inflammatory phenomenon that is still not well understood. It is treated medically and can last for several months (even years), requiring specific care with adapted rehabilitation, complementary testing and sometimes pain management. It is unpredictable in its appearance, its evolution and its potential consequences.
Nerve damage can occur due to the persistence of the inflammation, neuropathy of the posterior tibial nerve or due to wounding caused perioperatively due to adhesions.
Autres : Compartment syndrome, arterial vein wound, pyoderma gagrenosum…
Keywords:
Tarsal Tunnel – Compression of the internal plantar nerve or posterior tibial nerve—Neurolysis—Nevritis—Heel pain—Difficulty bending toes—Difficulty spreading toes—Achilles tendinitis—Plantar aponeurosis—plantar fascia —Foot cramps—Toe cramps—Calf cramps—Echo Doppler—Varicose veins—Phlebitis—Cotton feet—Loss of sensation in the foot—Algodystrophy—Fibromyalgia—Sever’s disease (calcaneal apophysitis).