procedure / elbow and shoulder Ulnar Nerve Compression Syndrome of the Elbow
Ulnar Nerve Compression Syndrome of the Elbow
Anatomy:
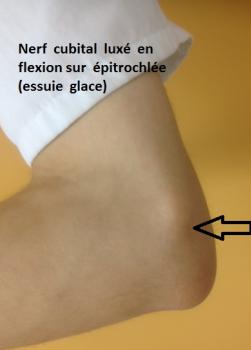
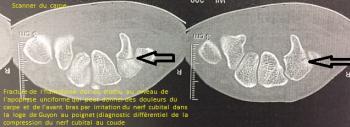
The ulnar nerve originates in the C7-C8-D1 roots and terminates in two branches. Along the way, there are many possible sites where compression can occur: spinal, cervico-thoracic, epitrochleo-olecranian and at the arcade of the anterior ulnar or deep aponeurosis of the forearm, Guyon’s canal.
The ulnar nerve is tense when the elbow is bent. It is stretched and must be able to slide (back and forth) easily to extend and flex. Thus, it is continually subjected to stretching on a regular basis, given the required use of the epitrochleo-olecranial ligament.
Description and Symptoms:
The following describes the tunnel syndrome due to compression of the ulnar nerve at the level of the elbow. This can lead to tingling of the 5th and 4th fingers (sometimes numbness, paresthesia, burning, a sensation of heaviness in the arm, pain under the arms or in the breast). This can also lead to a loss of sensation in these fingers and a muscular depression (muscle wasting) in the hand muscles (amyotrophy of the hand: “monkey hand”, paralysis of the 4th and 5th fingers, uncoordinated or painful fingers). This type of pain can be associated to elbow pain (cracking the elbow…) and shoulder pain, as well as pain in the arm or elbow and wrist, sometimes the shoulder (posterior or pain in the shoulder blades), neck pain (leading to pseudo-migraines) or eye socket pain. Indeed, shoulder-blade or scapula pain seem to be specific to a compression of the ulnar nerve in the elbow (See “Shoulder Pain and/or Scapula Pain and the Association with Compressive Nerve Syndrome” and other papers on this subject published in French: ”La douleur de l’épaule et/ou de la scapula et son association avec un syndrome compressif nerveux” P. Cottias, D. BIAU, Ph. Anract ; 90ème réunion de la SOFCOT, Palais des Congrès, Paris, November 2015 Paris ; Les signes atypiques de compression du nerf cubital» P. Cottias, A. Verlière, V. Boulier, JP. Mousseaux, Ph. Anract 90 ème réunion de la SOFCOT, E-Poster Palais des Congrès, à Paris novembre 2015 Paris).
It is also possible to have lesions from scratching or itchiness on the elbow or forearm that correspond to the nerve’s trajectory or another type of lesion (eczema-like in that the itchiness is associated with the carpal tunnel and ulnar nerve of the elbow as per a study of 26 patients we researched ("Le prurit et son association dans le syndrome du canal carpien et du nerf cubital au coude" - A propos d’une série de 26 patients- P. Cottias, D. BIAU, Ph Leclerc, Ph. Anract Journées Dermatologiques de Paris, (E-poster). Palais des Congrès, à Paris décembre 2016 Paris).
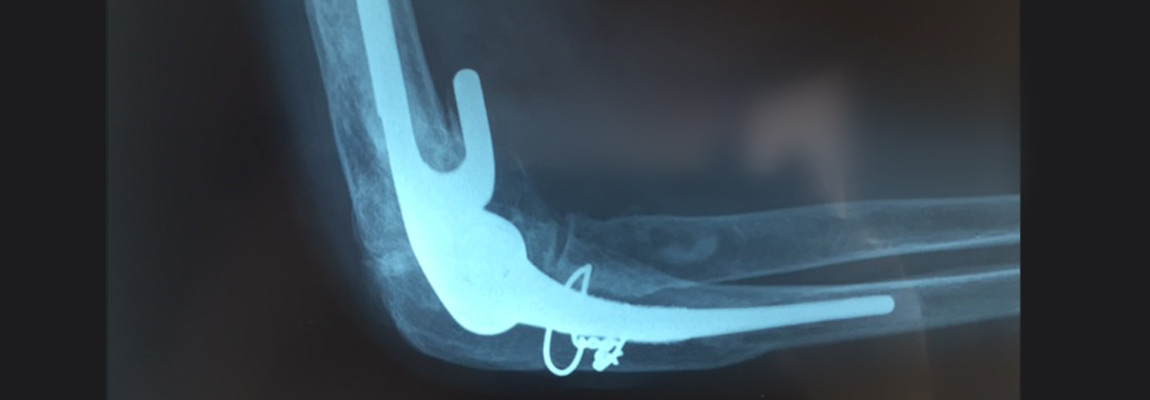
Likewise, other phenomena, such as trembling, can be linked to ulnar nerve compression (see the video on YouTube entitled: "Tremblement du poignet et des doigts"). If the ulnar nerve is affected, this can provoke extreme stiffness (blocages) of the elbow or shoulder (associated capsulite) even after a fracture has been operated on or treated or placed in a cast (radial head fracture, lateral coronoid process fracture).
Finally, pain, as with carpal tunnel, can also mimic cervicobrachial neuralgia (pain in the neck, shoulder, elbow, wrist and fingers).
The syndrome of the ulnar nerve is often related to a compression of the median nerve of the wrist (carpal tunnel).
Diabetes, thyroid condition, rheumatoid polyarthritis…all predispose to this syndrome.
Diagnosis:
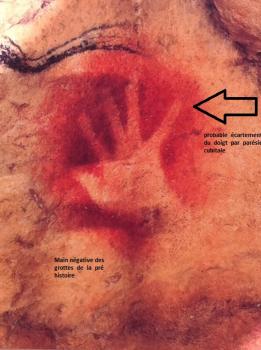
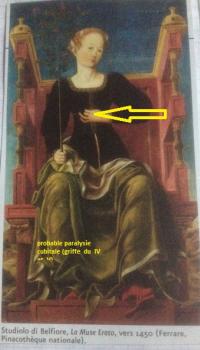
During the clinical exam, we can find electrical pain when percussing the elbow’s ulnar nerve in back of the epitrochlea (“irritable syndrome” or “Tinel’s sign”), a loss of hand strength, especially pinching between the index finger and the thumb, difficulty with fine motor gestures and electrical pain, a sensory-motor deficit with a loss of abduction-adduction of the fingers (“Watenberg’s sign”), trouble opposing thumb and fingers DIV (“Bourrel’s angle”) and trouble spreading one’s fingers (“the fan test”). Hand atrophy (disuse atrophy of the first interosseous muscle giving way to the “monkey-hand” deformity) and paralysis of the lumbrical muscles (ulnar claw, “claw hand” or “Spinster’s claw” with MP hyperextension and flexion of the IP). Finger flexion should not be confused with a bent finger due to retraction. The clinical examination can also reveal an associated compressed median nerve.
Standard elbow and cervical spine radiography is performed. An electromyogram (EMG) can confirm the diagnosis of the compression of the elbow’s ulnar nerve and specify the degree of severity by verifying whether or not the nerve is compressed in another spot as well. This exam can turn out to be normal (in 40 to 60% of the cases studied) but this does not, however eliminate the diagnosis. At this point, the physician will investigate a possible compression of the median nerve (often despite a normal EMG). A sonogram and MRI will also be useful for the diagnosis (inflammatory-white appearance, bifid median nerve, inflammation of the soft parts of the medullary bone on T2-weighted views on the MRI).
The diagnosis is ultimately a clinically-determined one, even if some complementary exams have negative readings. In fact, the patient in pain is often desperate when results of various exams turn out to be negative.
Treatment:
Without treatment, the ulnar nerve risks losing its capacity to function.
For early forms, medical treatment can be initiated: rest (sling-arm brace), infiltrations (corticosteroids at the elbow drain site) and rehabilitation therapy.
If medical treatment fails, surgery will be suggested.
Surgery is often performed under general or local/regional anesthesia.
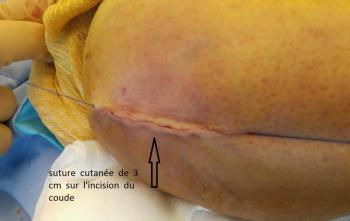
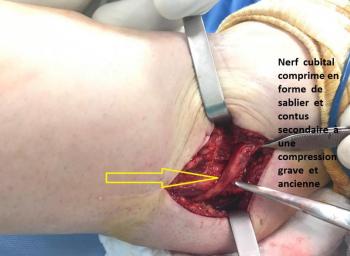
After the incision on the exterior edge of the elbow, centered on the ulnar nerve, the operation aims at decompressing the nerve at its three main sites of compression in the elbow. A bone graft may sometimes be necessary. Next, a transposition of the ulnar nerve is required. The ulnar nerve is displaced and set in front of the epitrochlea (medial epicondyle) and stabilized in a subcutaneous tunnel with a fatty flap.
Hospitalization & Recovery:
Hospitalization is ambulatory. The fingers and elbow are immediately mobile and aided by pain medication. The healing takes place over 10 to 15 days with the arm immobilized in a posterior sling, slightly bent, for 21 days.
The rate of progress is proportional to the severity of the pre-operative neurological affliction. In early forms, symptoms regress within several weeks. In more severe forms (conduction blockages visible on the EMG), tingling or a loss of sensation in the two fingers concerned may persist for some time and recovery is longer: 6 to 12 months.
A transitional period of reactive hypersensitivity can also be observed. Strength is often limited for several months.
Complications:
The most frequent are:
Hematoma: as with all surgery, there is a risk of hematomas that are generally absorbed on their own. On exceptional occasions, evacuating puncture or surgical drainage is necessary.
Algodystrophy (otherwise known as Complex Regional Pain Syndrome (CRPS) and Reflex Sympathetic Dystrophy Syndrome) is a painful, inflammatory phenomenon that is still not well understood. It is treated medically and can last for several months (even years), requiring specific care with adapted rehabilitation, complementary testing and sometimes pain management. It is unpredictable in its appearance, its evolution and its potential consequences.
Relapse is possible as long as neuropathy (deep anomalies of the nerve) continues.
The more rare are:
Deep infection is possible. It may require additional surgery and extended treatment with antibiotics. It is highly recommended not to smoke or consume unhealthy substances during the healing period as tobacco significantly increases the risk of infection.
Nerve damage to the ulnar nerve (caught in the fibrous scar tissue or a section of it) is exceptionally rare. However, a tingling sensation or loss of feeling to the two fingers concerned is frequent but recovery occurs progressively over a period of 3 months to 1 year. It is customary to say that during the first three months, no change between the pre-operative and post-operative condition can be observed. A transitional period of reactive hypersensitivity can also be observed.
Scars may remain swollen and sensitive, painful when touched for several weeks.
Temporary stiffness of the elbow can be observed and corrected with additional rehabilitation therapy.
Autres : compartment syndrome, phlebitus, pyoderma gangrenosum…
KEYWORDS:
Compression of the ulnar nerve – Carpal tunnel - pseudo Tinel – Monkey hand – Pain in shoulder blades or scapula – Breast pain - Elbow pain – Elbow stiffness – Blocked elbow – Shoulder and elbow pain - Wrist and elbow pain – Pain in the last two digits (4 and 5) - Watenberg - Bourrel’s angle – Fan Test– Conduction Block – Ulnar claw – Finger swelling - Burning fingers – Dead fingers – Cervicobrachial neuralgia– Electromyogram – Infilitration Test with Corticosteroids – Painting and the ulnar nerve – Spinster’s claw – shoulder capsulite - algodystrophy – fibromyalgia